Malaria is a deadly disease carried by mosquito bites infected with microscopic parasites. The mosquito inserts malaria parasites into your blood when it bites you. Rather than a virus or bacteria malaria is caused by parasites. Malaria can cause severe health problems such as convulsions, brain damage, difficulty breathing, organ failure, and death if not treated.
Malaria is a deadly disease carried by mosquito bites infected with microscopic parasites. The mosquito inserts malaria parasites into your blood when it bites you. Rather than a virus or bacteria malaria is caused by parasites. Malaria can cause severe health problems such as convulsions, brain damage, difficulty breathing, organ failure, and death if not treated.
Malaria is frequent in hot and humid tropical settings. In 2020, there were 241 million reported malaria cases worldwide, with 627,000 fatalities due to the disease. The vast majority of these occurrences take place in Africa and South Asia.
When a mosquito bites a malaria patient, the mosquito becomes infected. When that mosquito bites someone else, it introduces a parasite into its bloodstream. The parasites multiply there. Malaria parasites can infect humans in five different ways. Pregnant people with malaria can pass the sickness to their offspring before or during birth in rare situations. Malaria can be spread by blood transfusions, organ donations, and hypodermic needles but this is rare.
Plasmodium falciparum (P.f.) and Plasmodium vivax (P.v.), two of the parasite species that can cause malaria in humans, are the most dangerous. Malaria is caused by five different parasite species. Anopheles mosquitoes come in more than 400 different species, and about 40 of these are considered vector species because they can spread disease.
How Does Malaria Antigen Detection (Rapid) Test Diagnose the Disease?
Rapid diagnostic tests (RDTs) for the disease look for parasite antigens in human blood to diagnose malaria. For these tests, a drop of peripheral blood must be obtained, typically by pricking the fingertip or heel. Typically, visual read-outs are accessible in 20 minutes or less. Whole blood antigen for P.f. and P.v. malaria in one step to aid in the in vitro detection of malaria infection, the test quickly and accurately determines the presence of malaria antigen in human blood.
By allowing medical professionals to quickly discriminate between malarial and non-malarial fevers and choose the most suitable treatment, parasite-based diagnostic testing considerably lowers morbidity and death. It enhances patient care overall and may lessen the development and spread of medication resistance. It also helps patients with febrile diseases. When a quality-assured diagnosis is easily accessible, medical professionals should only treat patients who test positively for malaria; those who test negatively should have other possible reasons for fever investigated. Malaria Antigen Detection (Rapid) test are easy to use and gives results in 15 to 20 minutes.
Malaria is diagnosed using Malaria Antigen Detection (Rapid) Test. Early diagnosis and treatment of malaria typically result in complete recovery. Internal bleeding, renal failure, liver failure, and other potentially fatal consequences might result from malaria if it is not treated
Who needs Malaria Antigen Detection (Rapid) Test?
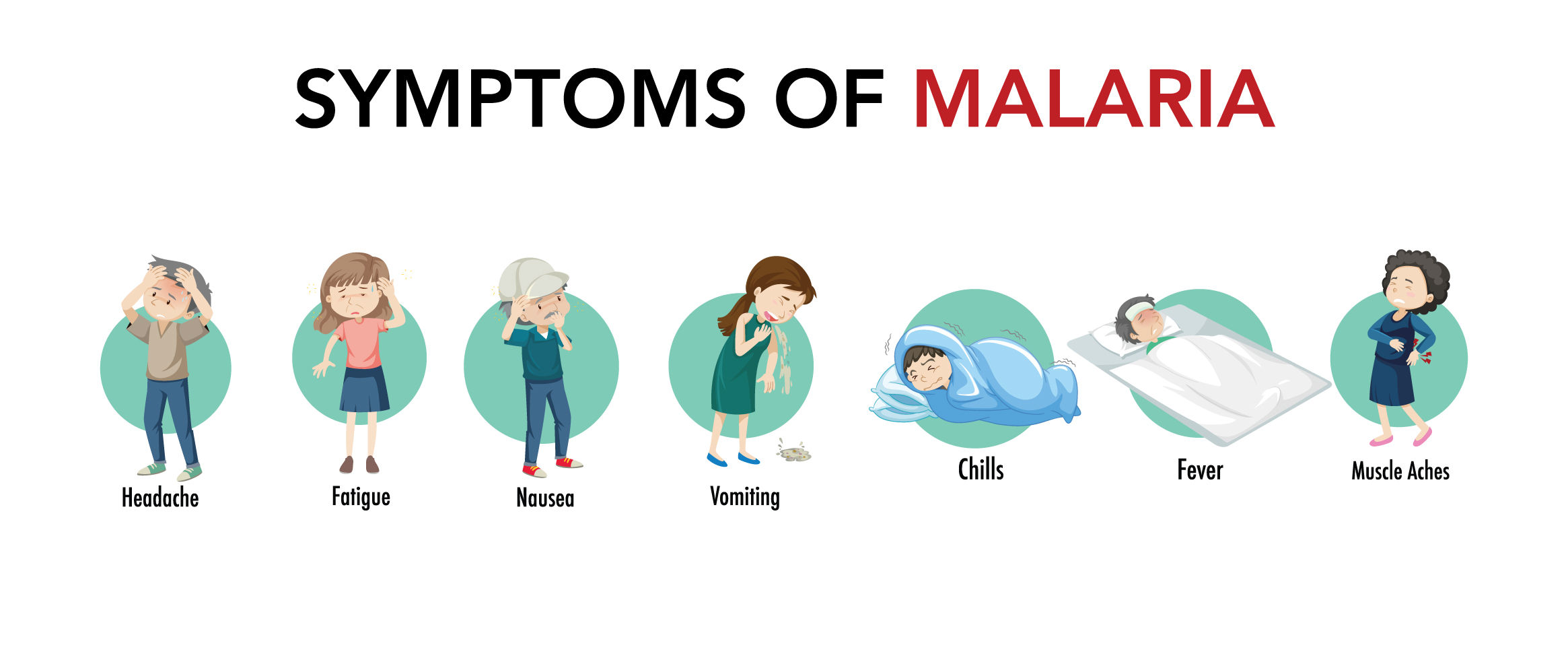
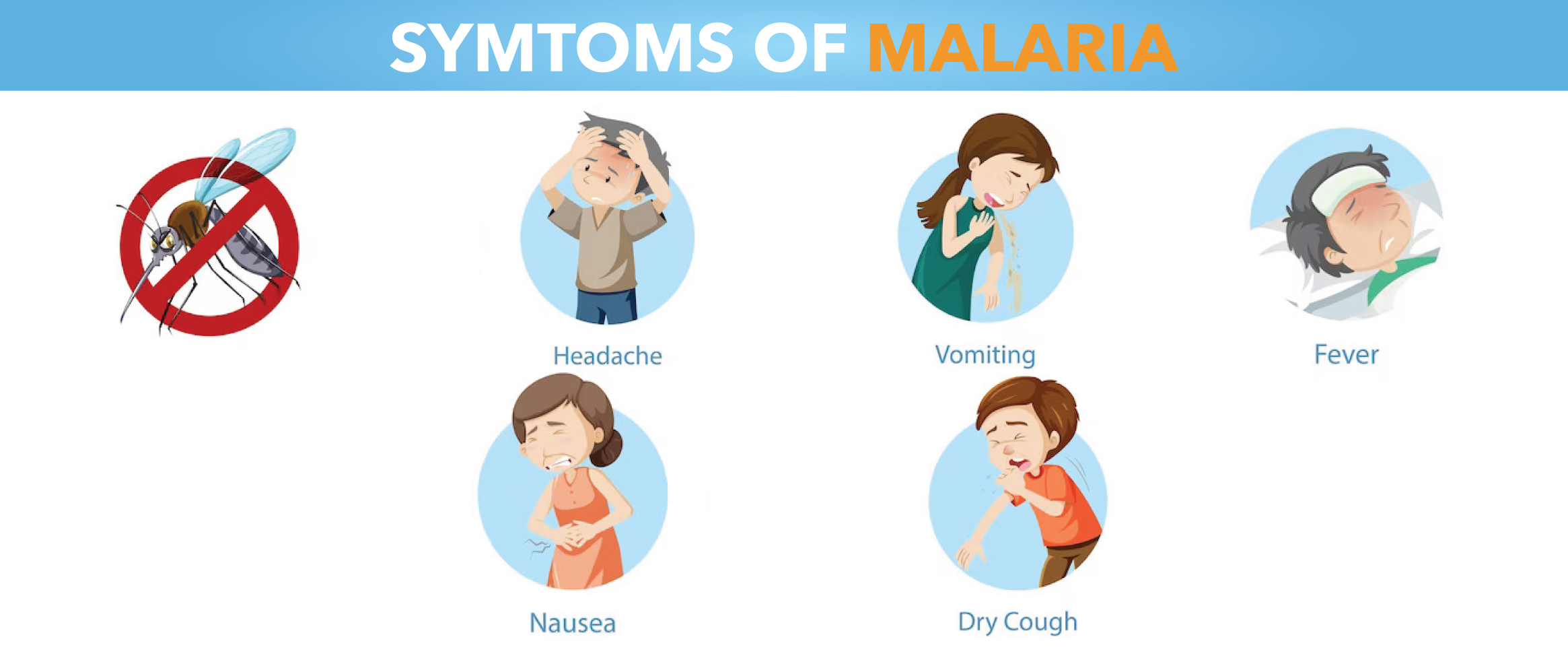
If you live in or recently returned from a region where malaria is prevalent and you exhibit malarial symptoms, you might need this test. The majority of people begin to experience symptoms 14 days after being bitten by an infected mosquito. However, symptoms may not occur for a year or they may take as little as seven days. Early signs of malaria infection are comparable to those of the flu and may include:
- Fever/chills
- Fatigue
- Headache
- Body pains
- Nausea and diarrhoea
The following symptoms may appear in the later stages of illness and are more severe:
- Extreme fever
- Severe chills and a shivering
- Tremors
- Soiled stools
- Yellowing of the eyes and skin called Jaundice
- Seizures
- mental haziness
How Malaria Antigen Detection (Rapid) Test is performed?
Your doctor will likely inquire about your symptoms as well as the specifics of your most recent vacation. Your blood will be checked to look for indicators of a malaria infection if an infection is suspected. One or both of the following tests could be performed on your blood sample.
- A blood Smear is taken on the slide.
- A drop of blood is applied to a properly prepared slide to create a blood smear.
- The slide will be examined under a microscope by a laboratory expert who will be searching for parasites.
- Malaria Antigen Detection (Rapid) Test. This test looks for antigens, which are proteins secreted by parasites that cause malaria. Although it can deliver results more quickly than a blood smear, a blood smear is typically required to confirm a diagnosis
- These malaria antigens are discovered in a person's blood by RDTs. A positive test result indicates that the person has malaria antigens. A negative test result would indicate that there are no malaria antigens present. Different RDT types can find various antigens.
Understanding of Malaria Antigen Detection (Rapid) Test results
- A Malaria Antigen Detection (Rapid) Test requires no particular preparation on your part. You could require retesting if your results were negative but you still have malaria symptoms. Malaria parasite counts can fluctuate from time to time. As a result, your doctor can ask for blood smears every 12 to 24 hours over the course of two to three days. To receive prompt treatment for malaria, it is critical to determine whether you have the disease.
- Your doctor will recommend medication to treat the condition if your tests were positive. Depending on your age, the severity of your malaria symptoms, and whether you are pregnant, the type of medication will be prescribed. Most instances of malaria can be healed if they are treated quickly.
Malaria Antigen Detection (Rapid) Test results interpretation
A line close to the letter "C" and a line close to the letter "T" indicates that the patient has malaria. The patient DOES NOT have malaria if there is a line near the letter "C" and no line near the letter "T." The test is invalid if there are no lines around the letters "C" and "T," respectively.
There have been reports of a 41–93% range in the sensitivity of AO staining for the detection of malaria parasites in infections with parasite levels below 100 parasites/l (0.002% parasitaemia). Excellent (>93%) specificity for P. falciparum infections, with the majority of observers recognizing the small ring forms.




 NABL approved
NABL approved  Most Trusted by
Most Trusted by  Accuracy &
Accuracy &  Widest Range
Widest Range